Potential Future Treatments
 PWS research is examining many aspects of the syndrome, looking to further understand symptom causes, develop new management strategies and find potential treatments.
PWS research is examining many aspects of the syndrome, looking to further understand symptom causes, develop new management strategies and find potential treatments.
Some of the latest research developments will be reported in the Research News section of our website, but information about some of the exciting, potential treatments raising ongoing, considerable hope can be found below.
Genetic Therapy and Reactivating the Silent Genes on the Maternal Chromosome 15 (updated Oct 2017)
Gene therapy alters DNA and remains an experimental technique in the world of medical research with very few treatments approved for medical use worldwide, but it is hoped that gene therapy techniques will be used in the future to treat disorders without the need for drugs or surgery. PWS researchers are actively investigating gene therapy to target mutated or defective cells and they are also attempting to reactivate genes on the maternal chromosome 15.

Dr Marc Lalande, creator of the world’s first PWS iPSCs (induced pluripotent stem cells.)
Normally, the paternal chromosome 15 has the set of genes linked to PWS switched on while the same set of genes on the maternal chromosome 15 are switched off. In PWS, those paternal genes are missing or unexpressed and patients only have the switched off genes from the mother’s chromosome 15. The idea of switching on the silent genes on the maternal chromosome 15 has been discussed and investigated for many years, but with the development of PWS stem cells in 2010 and the advanced knowledge of research teams, the possibility of this becoming a potential future therapy is starting to look much more promising. Activating these genes has the potential to restore normal cell function and might improve clinical characteristics. Several research teams are making exciting progress in this area: Dr Yong-hui Jiang’s team at Duke University, Dr Marc Lalande’s team at the University of Connecticut, Dr Robert Nicholls at the University of Pittsburgh and Dr David Segal at the University of California.
Dr. Yong-hui Jiang has screened thousands of drug compounds searching for small molecules that could activate PWS gene expression in cells derived from PWS mice and has found two compounds that seem to have this ability – UNC0638 and UNC0642. They then tested the compounds in skin cells from a person with PWS and observed activation of PWS-region gene expression, including expression of the significant SNORD116 gene cluster and the protein coding Necdin gene, to approximately 30% of normal. Following this success they treated PWS deletion mice for 5 days in their 2nd week of life with the low toxicity compound UNC0642. The mice exceeded usual life expectancy with improved growth and weight gain, and displayed normal appearance and activity. Theresa Strong, Director of Research at FPWR, suggests it’s possible these compounds or their derivatives may be tested on humans with PWS in the not too distant future, but she explains that this research leads to further questions about gene activation – when, where, how much, at what point during development does such a drug need to be given, how does genetic therapy of deletion vs. UPD differ, etc. Dr Jiang states “ Our study provides a critical step toward the development of a specific molecular therapy for human PWS. Based on these promising results, comprehensive evaluation of the efficacy and tolerability of G9a inhibitors in preclinical studies is warranted to fully explore therapeutic potential of G9a inhibitors for treating PWS.”
Dr Lalande’s team have identified a component of the switch off mechanism for silencing the PWS region on the maternal chromosome 15, a protein called ZNF274. They were successful in reactivating the PWS genes on the maternal chromosome by depleting and disrupting ZNF274 in PWS stem cells. However, ZNF274 also regulates other non-PWS genes, so interfering with ZNF274 can have unwanted consequences. Dr. Lalande’s group are now extending their work to develop a method that specifically disrupts the interaction of ZNF274 at the PWS region of the chromosome only, without affecting ZNF274 interactions with other regions of DNA. You can read more about this research here: “Therapeutic Potential of Blocking Zincfinger Protein 274 Binding To the PWS Locus.” and here.
Dr Robert Nicholls is using similar CRISPR genome editing technology to Dr Lalande to reactivate the silent PWS region genes with a focus on developing an approach that would recruit the cellular factors in order to keep the PWS genes active to induce long-term, stable PWS gene activation. Dr David Segal is reconfiguring engineered proteins to activate rather than repress genes as they were originally designed to turn off the maternal PWS region genes as a method to treat Angelman syndrome.
Dr Stefan Stamm at the University of Kentucky, known for his snoRNA work, and Dr Rudolph Leibel at Columbia University have been working in the field of genetic therapy to identify new therapeutic targets. Dr Leibel’s group were the first to generate hypothalamic PWS neurons (brain cells) in the lab and they have been investigating these neurons to understand how they function differently from typical neurons. Their work has led to a new understanding of the fundamental disruptions in PWS neurons and forms the basis for exploring new therapeutic targets that might correct the problems associated with PWS at a molecular biological level. These investigations have given rise to their breakthough discovery of PC1 deficiency.
PC1 – A New Insight and Therapeutic Target (updated April 2018)
Dr Rudolph Leibel, international obesity expert and co-discoverer of the leptin gene.
Drs. Leibel and Cole-Burnett at Columbia University published a study in 2016 that changed our understanding of PWS and opens up new avenues for therapeutic development. “This study changes how we think about this devastating disorder,” said Theresa Strong, PhD, chair of the scientific advisory board of the Foundation for Prader-Willi Research. “The symptoms of PWS have been very confusing and hard to reconcile. Now that we have an explanation for the wide array of symptoms, we can move forward with developing a drug that addresses their underlying cause, instead of treating each symptom individually.”
Drs Rudolph Leibel and Lisa Burnett made a breakthrough discovery that many of the neuro-hormonal abnormalities of PWS may be due to a deficiency of the enzyme prohormone covertase (PC1) in the brain. They discovered this by analysing PWS brain cells created using stem cell techniques. They also observed abnormally low levels of NHLH2, a protein which helps to produce PC1. To confirm whether PC1 deficiency plays a role in PWS, the researchers examined PWS mice (Snord116 deficient mice), finding them to be deficient in NHLH2 and PC1. As the function of PC1 is processing hormones and some of those are dysregulated in PWS (ghrelin, oxytocin, GHRH, and insulin), this discovery could be very important.
Dr Burnett believes the findings strongly suggest PCSK1 (the gene which makes PC1) and PC1 are good therapeutic targets for PWS. She states, “There doesn’t seem to be anything wrong with the gene that makes PC1–it’s just not getting activated properly. If we could elevate levels of PC1 using drugs, we might be able to alleviate some of the symptoms of the syndrome.” Following these findings, the Columbia research team began collaborating with Levo Therapeutics, a PWS-focused biotechnology company, to translate their research into therapeutics. Levo Therapeutics is a company formed by the parent of child with PWS, who also have the rights to develop Carbetocin (an Oxytocin-like drug in phase 3 trial) for PWS. You can read their press releases about PC1 on their website.
On the basis of Dr Leibel’s findings, Dr. Deborah Good, a NHLH2 researcher at Virginia Tech, is now researching how SNORD116 (critical gene cluster missing or deleted in PWS) regulates the NHLH2 and PCSK1 genes in a new study funded by FPWR. This project is called The SNORD116-NHLH2 Pathway: Insights Into the Molecular Genetic Basis of Prader-Willi Syndrome.
Hyperphagia / Obesity Drugs for PWS (updated March 2022)
 Weight loss drugs that are effective in the typical population have been found to have no effect in PWS. Developing a drug to treat the complexities of hyperphagia in PWS has been a challenge for pharmaceutical companies, but there are several drugs in clinical trial stages.
Weight loss drugs that are effective in the typical population have been found to have no effect in PWS. Developing a drug to treat the complexities of hyperphagia in PWS has been a challenge for pharmaceutical companies, but there are several drugs in clinical trial stages.
Exenatide and Liraglutide are both GLP Receptor Agonists, with the latter in phase 3 trial. GLP-1 is a gut derived hormone which reduces food intake and causes weight loss due to slowed gastric emptying and through direct central effects. There are some concerns around possibly slowing gut motility further, which can cause problems in PWS. Exenatide had some success in reducing appetite but without significant weight loss. Liraglutide (by NovoNordisk) is already FDA approved for improving glycemic control and reducing health risks associated with diabetes type 2, and whilst not funded in NZ, it is indicated to assist with weight management in obese adults by Medsafe NZ. Liraglutide is administered by daily subcutaneous injection and has recently been trialled in paediatric patients with PWS and obesity (but not diabetes) at various sites worldwide, including the Liggins Institute in Auckland. New Zealand’s trial investigator, Prof Paul Hofman, says that he has observed significant weight loss amongst patients he recruited. A results summary is yet to be published, but the trial is completed and result tables can be viewed.
DCCR (Diazoxide Choline Controlled Release) is thought to affect leptin pathways and improve GABA signalling. (Leptin is a hormone that helps to regulate energy balance by inhibiting hunger and its pathway is thought to be disrupted in PWS.) DCCR activates hypothalamic POMC neurons which signal to MC4 receptors to inhibit food intake and increase energy expenditure. It also inhibits NPY neurons, a regulatory peptide (associated with the GABA neurotransmitter), which have a role in stimulating food intake. The phase 2 trial results in PWS patients, presented here and here, observed a 35% improvement in hyperphagia with 4% reduction of body fat and about 5% increase in lean body mass, on average. There were also significant improvements in behaviours. In May 2018, Soleno Therapeutics (previously Essentialis) announced it is advancing DCCR into a phase 3 clinical development program (DESTINY PWS), receiving FDA Fast Track designation in July 2018. This phase 3 trial enrolled 127 patients and phase 3 top-line results were announced in June 2020. Unfortunately, the results did not meet statistical significance for primary endpoint of change from baseline in hyperphagia, but they did show significant improvements in a subgroup with severe hyperphagia. Significant positive changes were also seen in 2 out of 3 key secondary endpoints: improvement in Clinical Global Impression of Improvement score, and reduction of body fat mass measured by DXA scan. Unfortunately, the DESTINY PWS results were affected by the disruption caused by Covid-19 during 2020. To this date, participants of DESTINY PWS continue to receive DCCR in an extension study (C602), whilst Soleno continued to analyse old and new data and submit updated findings to the FDA in the hope of receiving an NDA (New Drug Application). The FDA had indicated that it is likely another trial would be needed, but in January 2022, following review of new data, the FDA suggested they were receptive to a study design involving participants currently enrolled in C602 to generate the additional control data necessary to support an NDA. Click to view further Soleno presentations.
Tesomet is a combination of tesofensine (a triple monoamine reuptake inhibitor) and metoprolol (a beta-1 selective blocker). Tesofensine blocks the reabsorption of 3 monoamine neurotransmitters: serotonin, noradrenaline and dopamine, increasing the levels of these neurotransmitters in the brain, which in turn reduces food cravings and appetite, and increases metabolic fat burn. It is being developed by Saniona who are recruiting for their phase 2b study taking place in multiple countries, including New Zealand. Phase 2a Step 1 demonstrated clinically meaningful weight loss (6.76%) and a statistically significant reduction in hyperphagia (43%) in adults with PWS at 0.5mg/day, but it was also discovered that plasma levels in PWS patients were higher compared to levels in non-PWS obese subjects, possibly causing the unwanted side effects observed. Therefore, a lower dose was recommended for adolescent PWS patients. Phase 2a Step 2 tested Tesomet in adolescents at lower dose (0.125mg) and was initially completed in January 2019, but a press release explained that a 24 week extension study was needed to obtain longer-term treatment data at a slightly higher dose for efficacy (0.25mg). Tesomet appeared to be well tolerated at lower doses. The phase 2b study aims to recruit 120 participants, aged 13-65 years (initially 18yrs+), who will randomly be given one of 3 different doses or placebo for the first 16 weeks. This initial period will be followed by a 36-week open-label extension where all participants will be treated with Tesomet at the highest tolerated dose as determined in the initial 16 weeks. Phase 2b is expected to be completed in December 2023. UPDATE March 2022: Unfortunately, Saniona have announced that they will be voluntarily pausing the Phase 2b clinical trials of Tesomet due to funding limitations. This is not related to the safety or efficacy of Tesomet. Saniona intend to continue evaluating strategic financing and business development options that could allow Tesomet to advance.
CSTI-500 is a triple monoamine reuptake inhibitor (similar to Tesomet), blocking the reuptake of serotonin, dopamine and norepinephrine. In phase 1 clinical trials it was found to be generally safe, well-tolerated and demonstrated weight loss effects that predict efficacy in patients. It is hoped that CSTI-500 will reduce symptoms of hyperphagia, obesity and behavioural issues such as social isolation, obsessive-compulsive disorder, cognitive disabilities and excessive daytime sleepiness. CSTI-500 is being developed by ConSynance Therapeutics and is phase II-ready.
Endocannabidoids – CB1R Blockers. The endocannabinoid system is a complex cell-signaling system involved in regulating processes such as appetite, metabolism, sleep, mood and pain. Endocannabinoids are molecules made by the body, similar to cannabinoids found in cannabis plants, which mainly bind to the CB1 or CB2 receptors. Endocannabidoids are thought to be involved with hyperphagia and the altered metabolism in PWS, but early trials in PWS with a CB1 Receptor antagonist, Rimonabant, were terminated due to psychiatric adverse events, although weight loss and reductions in body fat mass were observed. Investigators developed a new compound (JD5037) which would act peripherally (outside the brain) to block CB1 without causing behavioural effects. They tested JD5037 in Magel2-null mice and also measured circulating plasma levels of endocannabidoids in individuals with PWS. They found that eCB levels were significantly elevated in PWS and appeared to be correlated with the altered metabolic profile. JD5037 was successful in reducing body weight, hyperphagia and adiposity in PWS mouse models without affecting behaviour. This study demonstrated that treatment with a CB1R antagonist may be an effective strategy for the management of severe obesity in PWS. Inversago Pharma has developed a CB1 inverse agonist / antagonist compound, INV-202 for metabolic disorders, which also acts peripherally with CB1 receptors. A phase I study of INV-101 evaluated safety and tolerability, with encouraging INV-202 phase 1 results being announced in January 2022.
Cannabidoil (CBD oral solution) – RAD011
Unlike THC, Cannabidoil (CBD) is a non-psychoactive cannabidoid of the cannabis plant. It acts on cannabidoid receptors and it has the potential to address both hyperphagia and anxiety in PWS. A synthetic cannabidoil oral solution was developed for PWS by INSYS Therapeutics, but their phase 2 study examining its effect on hyperphagia-related behaviour was terminated early due to bankruptcy. However, the data was directionally supportive of reducing hyperphagia and there was a positive trend in reducing weight. The CBD assets of INSYS were acquired by Benuvia Therapeutics, and Radius Health acquired global development and commercialisation rights to Benuvia’s synthetic CBD oral solution, RAD011, in December 2020. RAD011 has demonstrated favourable safety and tolerability data, having been assessed in over 150 patients, and has FDA fast track designation. Radius are soon to start recruiting for their phase 2/3 trial, SCOUT-015, which aims to recruit 220 participants with PWS aged 8-65 years. The trial is expected to be completed in August 2024.
CBD oil is available to purchase in some countries, but is only available by prescription in NZ, at cost to patient.
Cannabidivarin (CBDV) is another non-psychoactive cannabinoid produced by the cannabis plant. It is very similar to cannabidoil, but appears to exert its effect on different membrane receptors. It is hoped that CBDV will address both hyperphagia and behaviour. Its efficacy and safety is being assessed for both ASD and PWS by Eric Hollander at Montefiore Medical Center. A phase 2 trial is currently recruiting participants with PWS aged 5 – 30 years.
ARD-101 is a gut-restricted, bitter taste receptor agonist that activates the secretion of gut peptide hormones, such as GLP-1 and GLP-2, which can lead to responses including appetite suppression, reductions in glucose and insulin, the lowering of LDL cholesterol, and an anti-inflammatory effect. It’s gut restriction enhances its safety profile. It is being developed by Aardvark Therapeutics and has shown good promise in preclinical studies (animal model). Aardvark CEO says ARD-101 “is differentiated from existing standard-of-care drugs in both its anticipated safety profile as well as its potential broad spectrum of effects….that impacts metabolic and inflammatory mediators.” A phase 2 study in a small group of patients with PWS aged 17 years+ is currently underway.
Oxytocin hormone treatment and Carbetocin, an oxytocin-like treatment, are also having positive effects on hyperphagia – read more by clicking the Oxytocin tab above.
A natural treatment being trialled for dietary management in PWS is caralluma fimbriata extract (CFE) which comes from an edible cactus plant and has been used for centuries in India as an appetite suppressant. Joanne Griggs found CFE to be effective in reducing hunger for her own child so conducted a study at Victoria University in Australia (involving some families in New Zealand) which saw an accumulative easing in appetite behaviour for one-third of the participants. Jo Griggs is happy to be asked questions about using CFE and can be contacted via email at joanne.griggs@live.vu.edu.au or jo@miaresearchfoundation.com
Treatments No Longer Being Developed for PWS
RM-493 / Setmelanotide is an MC4R agonist targeting the MC4 receptors which reside in the hypothalamus and promote satiety. (A defect in the MAGEL2 gene in PWS impairs POMC neurons which are key components of the MC4 pathway.) It was in trial for other genetic obesity disorders and has now been FDA approved for patients 6 years+ with obesity caused by POMC, PCSK1 and LEPR deficiency. It has also been granted PRIority MEdicines (PRIME) designation by the European Medicines Agency for the treatment of obesity and the control of hunger associated with deficiency disorders of the MC4 receptor pathway. The trial involving patients with POMC-Deficiency, a very rare genetic form of obesity where patients also suffer from dysregulation of the hypothalamus resulting in intense hunger and weight issues, achieved positive results with regards to weight and hunger, as well as a marked improvement in insulin resistance. Unfortunately, a phase 2 study involving PWS patients produced modest effects on reducing hyperphagia, but had no effect on weight, although there was some evidence of weight loss in the subset of patients treated at the highest dose level for the longest duration. Whilst Rhythm Pharmaceuticals focused setmelanotide development on 6 other obesity disorders, they were also assessing opportunities to further evaluate it in PWS, which may be in parallel or in conjunction with their acquisition of RM-853, a ghrelin o-acyltransferase (GOAT) inhibitor which was in preclinical development for PWS. To date, there has been no further public indication that studies involving PWS patients will take place, but preclinical development could be ongoing.
Beloranib and ZGN-1258 – Beloranib is a MetAP2 inhibitor and these have other uses, but when indicated for obesity, they work to re-establish balance to the ways the body metabolises fat. Beloranib was one of the drugs showing the most encouraging results so far for hyperphagia and weight loss, but was halted from further development after 2 trial participants sadly and unexpectedly died from blood clots in the lungs during its phase 3 trial. Zafgen, the company who were developing Beloranib, had since worked to develop other MetAP2 inhibitors which should not cause the same thrombosis risk, and in January 2018, Zafgen announced the selection of ZGN-1258 as their new development candidate for PWS. Unfortunately, despite promising initial results demonstrating positive effects on appetite, weight and behaviour in various mouse models of hyperphagia, obesity and PWS-like characteristics in preclinical development phase, ZGN-1258 was found to have toxic effects on muscle tissue and its development programme was suspended. This was the first time an adverse event of this kind had been seen with a MetAP2 inhibitor, so researchers believed the effect to be specific to ZGN-1258. Zafgen were committed to evaluating ZGN-1258 further and exploring other potential options within their portfolio of MetAP2 inhibitors, but the successive failures of Beloranib and ZGN-1258 ultimately led to a necessary merger with Chondrial Therapeutics to form Larimar Therapeutics. We are unsure if Larimar have plans to continue a MetAP2 inhibitor programme, and they have another drug focus at present. Principal Investigator, Shawn McCandless states, “Alternative MetAP2 inhibitors without an effect on thrombotic parameters, as well as the proteins whose actions are altered by MetAP2 inhibition offer promising targets for treating the hyperphagia and obesity in PWS.”
AZP-531 / Livoletide by Alize Pharma, is an unacylated ghrelin analog which aimed to target and inhibit the metabolic effects of abnormally high acylated ghrelin (‘hunger hormone’) levels seen in PWS. It was described as having encouraging phase 2 trial results for reducing hyperphagia symptoms and was developed by Millendo Therapeutics in a phase 2b/3 trial (ZEPHYR) which recruited 8-65 yr olds at various international locations. Despite promising initial expectations (here and here), Millendo decided to discontinue its Livoletide programme in April 2020 after Livoletide failed to significantly reduce hunger and improve food-related behaviours. It is thought that the abnormally high levels of ghrelin in PWS may just be a marker of hyperphagia rather than what drives it.
GLWL-01 by GLWL Research Inc. also aimed to target elevated acylated ghrelin levels by decreasing AG levels circulating in plasma. It had been successfully tested in patients with type 2 diabetes and was found to reduce AG levels at doses of 150mg+ twice a day. Significant decreases had been observed with higher doses and in phase 2, GLWL-01 was tested in PWS at a dose of 450mg twice a day in adolescents and adults 16yrs+ at multiple sites in the USA and Canada. The phase 2 trial was completed with results tabled in 2020 – no news has been posted publically, but development is believed to be halted due to lack of significant effect.
Summary of Oxytocin / Carbetocin Therapy Research for PWS to date (updated February 2022)
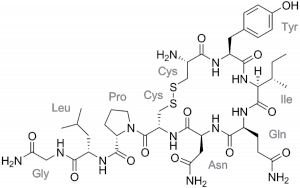
Oxytocin (OT) is a naturally occurring hormone released from the hypothalamus in the brain. It is associated with maternal care, bonding, feeding in infancy, social cognition, OCD, anxiety and appetite control. A reduction in the number of neurons that produce oxytocin and reduced oxytocin receptor (OTR) gene expression in PWS are believed to play a role in PWS psychopathology. It is suggested the disruption of oxytocin feedback in the hypothalamic paraventricular nucleus possibly influences vasopressin (AVP) signalling (another, related hypothalamic hormone). Use of OT administered via nasal spray as a therapy for improving behaviours is being actively studied in PWS and other conditions where altered OT pathways are associated with behaviour, such as autism spectrum disorder (ASD), Fragile X and Williams syndrome.
Oxytocin
Its potential as a treatment for PWS has generated much interest in the PWS community with an international fundraising effort taking place to specifically support the phase 2 oxytocin study by Drs. Jennifer Miller and Dan Driscoll at the University of Florida. However, early clinical trials of intranasal oxytocin in PWS produced conflicting results. The first, a pilot study by Dr. Tauber in France, 2011, trialled a single oxytocin dose in a small group of adults and observed a significant increase in trust and decreased sadness tendencies with less disruptive behaviour after 2 days. Hopes were raised that oxytocin may improve socialisation in PWS and longer term and dose-effect studies were recommended. A second study by Dr. Stewart Einfeld at The University of Sydney, 2014, looked at longer term treatment in adolescents and young adults. 30 families took part in this trial (including some from New Zealand), but the results found that oxytocin had little impact on any measure (behaviour, OCD tendencies, hyperphagia and sleepiness). An increase in temper outbursts was also observed with higher dose oxytocin. However, researchers have remained optimistic because oxytocin signalling is very complex and it is believed that finding the correct formulation and dose may be crucial to the success of oxytocin therapy.
A phase 1 study by Dr Miller et al at The University of Florida, 2017, trialled OT in 24 children (5-11 years) and the results were encouraging. Improvements were observed in behaviour, social responsiveness and hyperphagia. They concluded, “The results from this study suggest that low dose intranasal oxytocin is safe for individuals with PWS and may result in reduction in appetite drive, and improvements in socialization, anxiety, and repetitive behaviors. Further long-term studies with a larger population of participants are necessary to confirm these findings.”
A phase 2 randomised, double-blind 8-week study trialling intranasal OT (IN-OXT) vs. placebo in 50 children and adolescents (5-17) is due to be conducted by Dr Eric Hollander and his team at the Montefiore Medical Center, Albert Einstein College of Medicine in New York. After an initial pilot and refinement, this study is now recruiting. (The trial was originally planned to start earlier, but is now expected to be completed in Sept 2022.) They will be assessing affects of oxytocin on appetite, repetitive behaviours, weight and body composition, quality of life, and measuring salivary oxytocin and hormone levels (including ghrelin, pancreatic polypeptide, peptide YY, GLP-1, insulin, glucagon, testosterone, and estrogen).
Dr. Tauber and her team in France are also conducting a phase 2 trial by expanding their initial OT trial in adults for a longer duration trial with multiple doses and using advanced brain imaging analysis. They aim to find the optimal schedule and dose for adults with PWS. A trial outcome is yet to be published.
A phase 2 trial by Dykens, Roof, Miller et al, 2018 (sponsored by Ferring Pharmaceuticals) evaluated intranasal OT in a large group of children and adolescents (10-18) and was declared a success with clinically meaningful improvement in hyperphagia and associated compulsive behavioral symptoms compared to placebo. This trial is very interesting because a slightly different form of OT was used (FE992097) to specifically target only the OT receptor which may reduce impact on other systems, i.e. AVP signalling, therefore limiting any unwanted side effects. (In comparison, the initial studies by Drs.Tauber, 2011, and Einfeld, 2014, used Syntocinon, a synthetic substance identical to natural oxytocin.) The rights to this Ferring Pharmaceuticals oxytocin-like drug, Carbetocin, were purchased by Levo Therapeutics and renamed LV-101. A large scale phase 3 trial for LV-101 (CARE-PWS) recruited 7-18 yr olds at sites across the USA and Canada, with participants administering LV-101 three times daily before meals. Top-line results for CARE-PWS were announced in Aug 2020 and although the study did not meet its primary outcome measurements evaluating the 9.6 mg dose of LV-101, statistically significant reductions in hyperphagia and symptoms of anxiety and distress were observed with the 3.2mg dose, in which carbetocin was generally well-tolerated. More than 98% of CARE-PWS participants elected to receive the 3.2mg dose in long-term follow up and in extension periods. In July 2021, a New Drug Application for LV-101 was granted Priority Review by the FDA for the treatment of hyperphagia and behavioural symptoms in PWS, but ultimately, the review was unsuccessful as there were concerns about efficacy. This was a very disappointing outcome, especially considering the positive results observed and the combined efforts of families, FPWR and PWSA(USA) to support Levo’s application, which included compelling testimonies given by families at the review meeting. In January 2022, the FDA explained that, while LV-101 appears to be generally safe and well tolerated, the efficacy data available for the proposed 3.2 mg dose were insufficient and they recommended an additional clinical study be conducted to confirm results of this dose. Levo is currently in discussions with FDA regarding the design of this new study and continues to provide carbetocin to existing study patients. Levo Therapeutics is a company formed by the parent of child with PWS and is dedicated to advancing treatments for PWS and similar disorders. There is much excitement about Carbetocin because it was specifically designed to limit any potential unwanted side effects, it is well tolerated and it is the closest oxytocin-like therapeutic option to being approved for use in PWS. Carbetocin is approved in over 90 countries for uterine atony and postpartum haemorrhage (PPH), but this newer analogue of oxytocin is not yet used in NZ / approved by Medsafe.
Overall, Oxytocin studies are still experiencing mixed results. A 4-week, randomised, double-blind, placebo-controlled study in the Netherlands by Kuppens, Donze and Hokken-Koleaga, 2016, produced initially disappointing results with no significant improvements observed overall. However, when they examined age subgroups, they noticed there were positive results in some of the children younger than 11, with parents reporting significantly less anger, sadness, conflicts and food-related behaviour, and improvement of social behaviour. Their study had involved participants age 6-14 years and they concluded, “This study suggests that intranasal oxytocin administration has beneficial effects on social behaviour and food-related behaviour in children with PWS younger than 11 years of age, but not in those older than 11 years of age.” A similar follow-up study by The Dutch PWS Reference Centre, published in 2020, trialled a slightly lower dose in children 3-11 years for 3 months and the results were interesting because OT was found to have positive effects on social and eating behaviour in 3-11 year old boys with PWS and in children with a deletion, but no significant effects in the study group overall.
There is still much to learn about oxytocin levels in PWS, the genetic variability of the oxytocin receptor gene, the impact of the OT system on the developing brain in PWS and why there are variable responses to oxytocin. Researchers believe we need these answers in order to effectively calculate dose and the optimal age for treatment. In 2015, FPWR funded further oxytocin research by Dr. Stewart Einfeld’s team in Sydney. One study aims to understand the true nature of the oxytocin abnormality associated with PWS which will help direct oxytocin or vasopressin interventions. They intend to discover if there are similarities with the reduced levels of 9-amino-acid active oxytocin and increased extended oxytocin found to be present in people with ASD. They also intend to find out more about the hypothesised suppressed oxytocin receptor which could make the OT system inactive, even when high levels of OT are administered. It’s possible that vasopressin receptors may be responding to administered oxytocin so they will measure plasma levels of the two forms of oxytocin vasopressin and DNA levels of the oxytocin gene. Dr Einfeld and his team are currently recruiting patients with and without PWS ages 13-30 years. A second study will investigate potential respiratory sinus arrhythmia abnormalities in PWS and how they may relate to emotional and behavioural problems and oxytocin / vasopressin abnormalities. Another FPWR funded study, by Dr Driscoll at the University of Florida, aims to evaluate factors that may affect the efficacy of intranasal oxytocin treatment in PWS. Dr Driscoll has noted that the genetic background of individuals is likely to impact how an individual responds to oxytocin therapy – this work needs further funding and development. At Harvard University, Dr Scammell explored the wake promoting effects of oxytocin and found that enhancing the activity level of the oxytocin system may indeed help maintain wakefulness in PWS.
Research in France has focused on early alterations from birth in the OT system and pathways of OT receptors in the perinatal period. In 2015, a French research team led by Dr. Meziane published results of a study examining the OT system in mice deficient in Magel 2 genes (deficient genes associated with both PWS and autism, causing deficits in social recognition, interaction and a reduced learning ability) and found modifications of the OT system that change from birth to adulthood. Daily administration of OT in the first postnatal week was sufficient to prevent deficits in social behaviour and learning abilities in adult males, and partly restore a normal OT system. FPWR funded a study by Dr. Muscatelli to further understand the relationship between the inactivation of Magel 2 and the alteration of the OT system and to investigate how an administration of oxytocin acts during brain development to allow a long term effect in Magel 2 deficient mice. This study aimed to increase knowledge about adequate supplemental therapy in infancy and provide insight into effective OT administration at different points of the OT system maturation (infancy to adulthood). Interesting findings were published in 2021, ‘The Impact of Oxytocin on neurite outgrowth and synaptic proteins in Magel2-deficient mice‘.
An exciting discovery by Dr Tauber and her team in 2017 confirm and extend the findings of Dr Meziane. They found that oxytocin improves feeding and social interaction in infants with PWS. 18 infants (age 3 wks to just under 6mths) were given oxytocin doses on different schedules and regardless of dose, all of the babies showed improvements in feeding skills with 88% being normalised after treatment. Some aspects of social behaviour also improved – measured facial expression, eye contact and interaction with parents. Brain scan images also revealed improved connectivity in the OFC brain region which is involved in emotional decision making. It is not yet clear if there is a long term impact of this early treatment and whether oxytocin has a ‘rescue’ effect, but this is an area of interest for further study. Another French study published in 2020 confirmed that OXT promises to have therapeutic benefit for modulating the sensory-motor reflexes necessary for suckling in infants with PWS.
It is hoped that the combined knowledge gained from these past and ongoing trials will refine understanding of the potential for oxytocin therapy and determine most effective use of oxytocin in children and adults with PWS. If benefit is clearly proven, multiple trials confirming this will help support approval (and the subsequent funding) of oxytocin for PWS in New Zealand. It is important to note that trials are in early stages and we forward caution about purchasing and using available forms of oxytocin before more is known about dose and safety.
Brain Stimulation as a Therapeutic Option
An alternative to using drugs as therapeutics is the use of devices to stimulate brain activity in specific regions. Two approaches experiencing notable early success are transcranial direct current stimulation (tDCS) and vagus nerve stimulation (VNS).
 Transcranial Direct Current Stimulation (tDCS) – 2017
Transcranial Direct Current Stimulation (tDCS) – 2017
tDCS has been used for treating depression and other mental health conditions with external electrodes transmitting a weak electrical current into the pre-frontal cortex area of the brain. Preliminary data in 5 adults with PWS showed some reduction in hyperphagia symptoms so Dr Merlin Butler and his team at Kansas University conducted a further study involving 10 adults with PWS, plus obese and healthy weight controls. Positive results were seen so Dr Butler is now collaborating with Harvard University to continue an expanded study to further determine if tDCS improves food cravings and overeating in adults with PWS. The project will enroll 40 adults with PWS and a variety of measures will be used from hyperphagia questionnaires to tracking eye movements and measuring brain wave activity. tDCS may be an effective, non-invasive and cost-effective therapy for food behaviour in PWS.
Vagus Nerve Stimulation (VNS) – 2017
Dr. Tony Holland and his team at the University of Cambridge have been using a slightly more invasive approach with a device requiring surgical implantation. Once inserted, the device can be turned on and off by an external control. Their preliminary study of 3 patients suggests improvements to maladaptive behaviours, temperament and social functioning. Dr Holland and his team are conducting a larger follow up proof of concept study with external (rather than surgically implanted) vagus nerve stimulators which have since become available in the UK.
t-VNS update – 2019
The proof of concept study results revealed, “4 of the 5 participants who completed the study exhibited a statistically significant reduction in number and severity of temper outbursts after approximately nine months of daily four-hour t-VNS.” Treatment was found to be safe and effective. This study used t-VNS (transcutaneous vagus nerve stimulation) where an external device was worn in the left ear so that an electrode could stimulate the auricular branch of the vagus nerve.
Success has been associated with increased activation of neurotransmitter systems and in particular, increased brain levels of gamma-aminobutyric acid (GABA), a neurotransmitter which is known to be reduced in some people with PWS.
A large-scale study is being planned to take place at multiple sites across the USA, funds permitting.
Pitolisant (updated Feb 2022)

Lara Pullen, PhD immunologist and freelance medical writer interested in systems biology, particularly the intersection of the immune, nervous, and endocrine systems.
Parent of a child with PWS, immunologist and co-founder of The Chion Foundation, Lara C. Pullen, PhD, identified pitolisant as an ideal drug to be repurposed to treat many clinical manifestations of PWS. The following, ‘Why Pitolisant?’, is from the Chion Foundation website, Dec. 2016.
“While originally identified as a key immunological molecule in the allergic response of humans, histamine is actually an evolutionarily-primitive molecule that plays many fundamental roles across many animal phyla. Humans possess four histamine receptor subtypes: histamine 1 receptor (H1R) through the histamine 4 receptor (H4R). The H3R drew our attention because it appears to achieve its homeostatic function via regulation of the release of various neurotransmitters including serotonin, acetylcholine, and dopamine.
If H3R were a critical receptor in the pathophysiology of PWS, this would explain why it has, to date, been difficult to identify a satisfying single genetic cause for PWS. While the role of the H3R has not yet been studied in PWS, research has revealed dysfunction in neurotransmission in patients with PWS. Specifically, the serotonergic system and, possibly the dopamine system, appear to be compromised in individuals with PWS. Dopamine is also known to play an important role in feeding and satiety. We note that the neurotransmitters that are dysregulated in individuals with PWS are those that are regulated by the H3R. The histamine h3 receptor is located in the brain and gut, and is known to regulate not only sleep/wake states, but also hunger, cognition, and movement, all of which are debilitating problems for patients with PWS.
Since the H3R is able to modulate other neurotransmitters, H3R ligands are being investigated for the treatment of various conditions and there are multiple H3R inverse agonists/antagonists in development. Multiple studies lend credence to the neuroprotective effects of this class of pharmaceuticals. The H3R inverse agonist pitolisant is newly approved in the European Union for the treatment of the rare sleep disorders of narcolepsy and cataplexy.
While improved wakefulness alone would be a major improvement in the quality of life of individuals with PWS, there are many reasons to believe that the neurologic benefits of pitolisant in the PWS population might extend beyond improving wakefulness. For example, mental health issues and learning disabilities could potentially be improved by pitolisant. Moreover, research suggests that the cognitive enhancing activities of drugs such as pitolisant may help protect against schizophrenia, attention deficit disorder, and other cognitive disorders. Lastly, children with PWS are often plagued with severe gastrointestinal problems that remain difficult to treat. Pitolisant may affect multiple cells in the gastrointestinal tract and could theoretically improve these symptoms. For these reasons, we propose that it is biologically plausible that pitolisant would be useful for the PWS patient population, not only in the treatment of excessive daytime sleepiness, but that it could also improve the ability of individuals with the syndrome to respond to environmental stressors such as changes in temperature, high glucose loads, and complex social interactions.”
As pitolisant was not available in the USA, the Chion Foundation have helped families trial this drug under a personal importation scheme. Seven families affected by PWS were prescribed pitolisant and documented their experience on TREND Community via journaling and survey questions. Caregiver data suggested “pitolisant is well tolerated and has neurological benefits that extend beyond wakefulness to include mental clarity, increased processing speed, improved attention, and improved muscle tone. Early patient experience with pitolisant is encouraging.” Chion Foundation partnered with Trend Community, an innovative patient experience and engagement platform, to launch the Pitolisant Health Initiative to explore the potential of pitolisant. In October 2017 Harmony Biosciences announced its licensing agreement with Bioprojet Pharma to bring Wakix (pitolisant) to market in the United States. “The Chion Foundation and Trend Community intend to continue its collection of patient experience data and work with Harmony Biosciences to secure an indication and label expansion for pitolisant for patients with PWS.”
In 2018, Pitolisant became available in the USA under an expanded access program and then received FDA Breakthrough Therapy Designation. Dosing data from 9 children treated with pitolisant was presented at the FPWR annual research symposium. In 9 children, benefits were observed at a higher dose than is usual for treating narcolepsy, although a tenth child had to stop treatment due to side effects. Detailed data was presented for 3 children and it was reported that they experienced improved mental clarity and processing speed. These 3 children had previously been frequently sleepy during the day, as is typical of many children with PWS, but they did not present with typical adult symptoms of narcolepsy which led to the conclusion that individuals with PWS, with and without a diagnosis of narcolepsy, may benefit from pitolisant.
In April 2019, the case series data from these 3 children was published. It was noted that the treatment was well tolerated and in addition to the positive effects on cognition, pitolisant had the additional benefit of normalising the children’s relationship to food. You can read more details about the dosing and any side effects in The Chion Foundation’s April press release. In May 2019, The Chion Foundation released this short film about patient experience with pitolisant. Later in 2019, pitolisant received FDA approval for narcolepsy, like its existing approval in the EU.
In 2021, a double-blind, placebo controlled phase 2 study was launched to evaluate pitolisant for excessive daytime sleepiness, cognition, and behavioural function in PWS, enrolling patients 6 – 65 years at various sites across the USA. Patients will be randomised to 3 different doses during the trial period and then have the option of participating in an open label extension. This study is still recruiting.