New area of the brain identified for developing therapeutic targets to manage hyperphagia
NOV 2021 – The hypothalamus and hindbrain have previously been implicated in appetite regulation, but drugs targeting these areas have not been as successful as hoped.
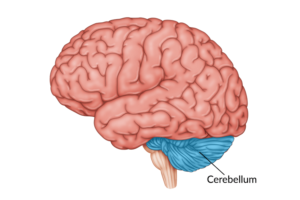 Dr. J. Nicholas Betley, of the University of Pennsylvania, and Dr. Albert Chen, of the Scintillon Institute, speculated that the cerebellum could play a role in hunger suppression and reached out to Laura Holsen, who had a rare set of data containing functional MRI scans from PWS patients. When reassessing the data, looking for differences in how the brains of PWS patients responded to food compared to a control group, the cerebellum stood out. They were able to identify and characterise a subset of glutamatergic neurons in the anterior deep cerebellar nuclei (aDCN) that were associated with promoting satiety.
Dr. J. Nicholas Betley, of the University of Pennsylvania, and Dr. Albert Chen, of the Scintillon Institute, speculated that the cerebellum could play a role in hunger suppression and reached out to Laura Holsen, who had a rare set of data containing functional MRI scans from PWS patients. When reassessing the data, looking for differences in how the brains of PWS patients responded to food compared to a control group, the cerebellum stood out. They were able to identify and characterise a subset of glutamatergic neurons in the anterior deep cerebellar nuclei (aDCN) that were associated with promoting satiety.
In experiments with mice, they found that activating these aDCN neurons led the mice to dramatically curb their meal size. Interestingly, the researchers discovered that the mice would stop eating when their calorie intake was sufficient, but if they were given less calorie dense food, they would eat larger quantities to ensure appropriate calorific intake. Then, they looked at how activating these neurons interacts with reward circuits known to influence eating and found that they affected dopamine reward pathways in the brain’s ventral striatum by increasing striatal dopamine levels. They believe that long-lasting increases in baseline levels of dopamine may reduce the rewarding effect of food.
Finding ways to turn these aDCN neurons on and off in people with PWS would be an exciting next step. We hope to be able to follow clinical studies involving patients with PWS to see how this works.
Pennsylvania Today Article: https://penntoday.upenn.edu/news/brains-cerebellum-new-target-suppressing-hunger