Hypothalamus analysis characterized by neuronal loss, altered neuro-plasticity and neuroinflammation – a potential role for BDNF identified
MARCH 2018 – For cell building and maintenance, DNA ‘instructions’ are ‘read’ and transcribed into RNA and these ‘read-outs’ are called transcripts. A transcriptome is the complete set of RNA transcripts that are produced by the genome (all the genetic material in a cell). In this study, transcriptomic analysis of hypothalamic PWS brain tissue by RNA sequencing was performed. Altogether, 3676 differently expressed genes were identified. The analysis identified a transcriptomic signature characterised by neuronal loss, neuroinflammation, and altered neuroplasticity (ability of the brain to adapt, remodel or optimise neural networks.)
Previous neuroimaging studies and case reports in PWS have identified structural abnormalities that would be consistent with a reduced number of neurons, such as reduced grey matter volume in a number of cortical areas and abnormal gyrification (process of forming the folds of the cerebral cortex.) The analysis found that upregulated genes (increased receptors / cellular response) overlap with the transcriptome of leptin-responsive mouse AgRP neurons (neuropeptide produced in the brain) that signal hunger, while downregulated genes (decreased receptors / cellular response) overlap with the expression profile of POMC neurons (a precursor polypeptide) activated by feeding.
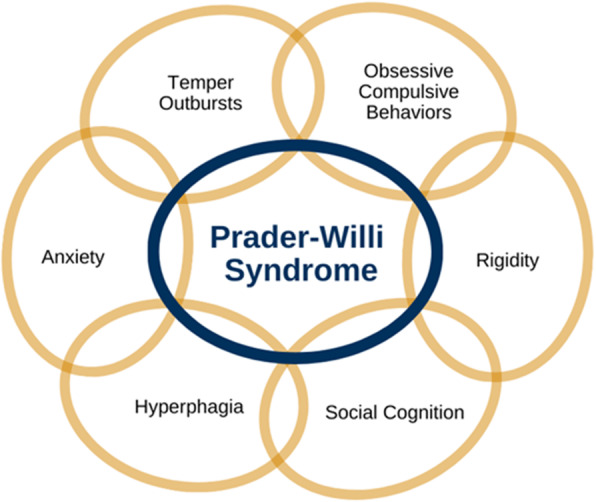
Researchers also suggested a potential role for BDNF (brain-derived neurotrophic factor) in downregulating genes in PWS which requires further exploration and may have therapeutic relevance. In mice and humans, genetic disruption of BDNF causes developmental delay, stereotyped behaviours, impaired pain sensation, hyperphagia, and severe obesity – characteristics that show some overlap with those seen in PWS. Fluorescence in situ hybridization of human hypothalamic tissue suggested that the number of cells expressing BDNF was reduced in the ventromedial nucleus of the hypothalamus in PWS, but the researchers measured levels of plasma BDNF in patients with PWS versus age-matched obese controls, but did not find a significant difference. Possible explanations are that BDNF levels are known to vary considerably in plasma versus serum and among assays; additionally, plasma BDNF may not reflect BDNF expression in the brain. This study also found a low level of oxytocin mRNA and a smaller number of cells immunoreactive for oxytocin in the paraventricular nucleus in PWS samples, supporting previous findings and the key role of oxytocin, as well as BDNF, in the neuropathology of PWS.
Additional studies are needed to replicate these findings and to investigate the potential loss of other neuronal populations (including POMC and AgRP neurons) within the hypothalamus in PWS. Cumulatively, these data identify a transcriptomic signature in PWS consistent with marked hypothalamic neurodegeneration, which may be mediated in part by reduced expression of the neurotrophin BDNF and its receptor, TrkB.